Adding what we can to life:
Treating rheumatoid arthritis,
and fighting medical arrogance
By Dr. Stephen R. Keister / The Rag Blog / January 5, 2011
[Dr. Keister’s lastest dispatch is, in part, a response to David P. Hamilton’s December 15, 2010, Rag Blog article, “My Remission and the Business of American Medicine.” Dr. Keister is himself a retired rheumatologist.]
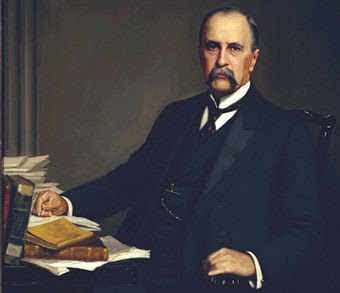
Sir William Osler once observed, “We are here to add what we can to life, not to get what we can from it.”
I now will deviate from my usual rantings about the inferior state of medical care in the United States, and the sociological and political implications of same, and take a look into the actual practice of clinical medicine.
There is among many physicians in the United States an arrogance that is difficult to understand. We who were informed by Dr.Osler’s thinking and consider our mission to be caring for the sick are angered when we read the kinds of things reported by David P. Hamilton in his article, “My Remission and the Business of American Medicine,” published recently on The Rag Blog. It is a revealing article by an intelligent, inquisitive academic who found all manner of problems when he was diagnosed with “rheumatoid arthritis.”
I feel that the essence of David’s problem, which surely was not of his making, is described in the fourth paragraph of his article:
The diagnosis of RA is not made in a casual manner. It is quite “scientific” (quotation marks are mine) and quantifiable on the basis of a blood test to determine your “rheumatoid factor.” For men, above the score is positive. At one point I was 176. Once you’re positive, it is “standard medical practice” to never test for that factor again, based on the assumption that the disease is always chronic, so further tests would be superfluous.
I say “poppycock”: The various types of arthritic diseases, and there are over 100 entities, or subsets, are largely diagnosed by listening to the patient, questioning him/her, and doing a detailed physical examination. We are currently caught up in a culture that encourages our seeing as many patients per day as we can, and attempting to allow the laboratory or radiology departments to make the diagnosis.
Let me go back to the days when we were treating ailing human beings and not practicing production line medicine under the oversight of the health insurance cartel and our financial adviser.
First of all, any rheumatologist should be versed in the writings of Dr. Hans Selye about the effect of “stress” in the production of disease. Selye defines “stress” broadly as an initiating factor in any number of illnesses. He is not referring to what we currently think of as emotional stress and I would suggest that those interested can find his voluminous writings by Googling his name. If he were to comment on the excellent exposition in David Hamilton’s article, Selye would reference a total hip prosthesis as “stress.”
I practiced rheumatology for 40 years and found that I could be 90% sure of an individual’s diagnosis after the initial hour’s interview. Then, and only then, would we undertake basic testing to confirm, or deny, my initial impression.
For instance a lady, aged 33, appeared with a history of generalized joint aching for the past several months. She was stiff upon arising in the morning. There was general fatigue and loss of grip strength. There was swelling of her knuckles and the first joints of her hands. (Merely observing the hands during the interview was a great help in the diagnosis.) She noted that her wrists and knees would swell at times and that there was tenderness of the balls of her feet. After a complete physical examination, including checking mobility of the various joints, one could pretty well conclude that this lady had early RA.
What then?
Basic laboratory work was ordered, including a complete blood count since anemia can accompany RA. The rheumatoid factor in most instances would be positive, BUT in a small percentage of cases could be negative — the so called “seronegative RA.” After basic clinical lab studies to ascertain kidney and liver function come the treatment phase.
Then we would discuss at length the implications of the disease and the prognosis, informing the patient that a certain number of folks would go into spontaneous remission after a length of time. We discussed the various facets of treatment, the non-steroidal anti-inflammatory drugs — or, rarely, short term corticosteroids — for relief, and in my latter years of practice methotrexate to try and induce remission. In the case of an especially painful joint we could inject it with medrol after freezing the skin with ethyl chloride.
As few words about methotrexate since Hamilton discussed it in his article. Methotrexate was originally an anti-cancer medication, but certain researchers felt it might help the skin condition psoriasis, which indeed it did, and concurrently gave great relief to the arthritis than may accompany psoriasis. Thus, certain rheumatologists, including The Cleveland Clinic (and I was among them) began to judiciously use it to treat RA. On a reasonably small dosage, given once a week, most patients began to experience relief within 1-2 months. It frequently would bring about early remission.
Before starting treatment with the drug we had a long discussion with the patient about the need for certain changes in lifestyle, including no alcohol use, and we educated the patient about warning signs for side effects, and the need for certain laboratory studies once a month to check for changes in blood count or liver function.
Each patient that started the medication was given detailed written instructions as well as an Arthritis Foundation booklet describing their specific arthritic disorder. Regular follow-up appointments were made and the patient was instructed to call if experiencing problems or having questions. I would point out that complications are much more common with the non-steroidal anti-inflammatory drugs than with judiciously used methotrexate.
Rheumatoid arthritis is statistically much more common in younger women than men. There is a variant known as Polymyalgia Rheumatica, usually seen after the age of 70 — and though also more common in women, it is much more frequently encountered in men than is RA. The onset of this condition is relatively sudden, with multiple joint involvement, with swelling and pain, but here there is much less tendency for the joints to swell or deform.
Fatigue is common. Headache may be a concurrent symptom since half the patients have concurrent inflammation of the artery in the temple. The physician must be alert to this because temporal arteritis causes blindness in certain individuals. The laboratory test that tends to confirm the diagnosis is a high sedimentation rate (over 100). The rheumatoid factor is USUALLY not positive but may be positive in certain instances. The disease is usually self-limited, 1-2 years in duration, and is followed by complete remission.
PMR is usually treated with low-dose prednisone since prednisone will usually abort the temporal arteritis. If the dose is low enough, over a limited period of time, the patient will be able to avoid the often frightening side effects of high dose prednisone therapy. Again, this must be discussed in detail with the patient, with reading matter provided, and regular follow-up arranged.
I could go on forever discussing systemic lupus, scleroderma, ankylosing spondylitis, psoriatic arthritis, degenerative arthritis, etc. If interested, the reader can find detailed and reliable information on the website of the Arthritis Foundation. The main point I want to get across is that a conscientious physician will devote an adequate amount of time to the patient, and will discuss in detail the type of arthritis involved and its treatment. We are here to provide relief, both physical and emotional, and not to be “pure scientists.”
Another saying of Dr.Osler: “There is no more difficult art to acquire than the art of observation, and for some men it is quite as difficult to record an observation in brief and in plain language.”
As my regular readers well know, I believe that responsibility for the deterioration of medical care in this country does not lie solely with the physicians, but much of the problem stems from a societal loss of vision. The underlying problem in our culture is worship of the golden calf, the desire to make money regardless of the costs to our neighbors.
The co-opting of the medical profession by the health insurance cartel has transformed many physicians into little more than businessmen. With our government dominated by the corporations and their prostituted legislators in Washington, with a mainstream media that pays deference to the powers that be, and a disinterested public that listens to and accepts propaganda and then votes against its own best interests, I can see little hope.
Meanwhile, while realizing that we can expect little more than cursory medical care for ourselves, we must continue to remember the 50 million of our citizens totally without medical care. We cannot spend our resources on empire-building and still be prepared to provide for the welfare of our citizens.
I wish to extend thanks to the editors of ProPublica for their extensive and excellent reporting of pharmaceutical company financial infiltration of the medical profession and of the medical schools. Please check out “Dollars for Docs: What Drug Companies are Paying Your Doctor” and “Med Schools Flunk at Keeping Faculty Off Pharma Speaking Circuit.”
And finally, our absurd approach to health care and other social issues is made abundantly clear in two other recent articles: “America in Decline:Why Germans Think We’re Insane” from AlterNet, and an excellent piece from The Independent also published on The Rag Blog, “Cuban Medics in Haiti put the world to shame.”
I join with all the Rag Blog community in hoping for a reasonably healthy and sane New Year.
[Dr. Stephen R. Keister lives in Erie, Pennsylvania. He is a retired physician who is active in health care reform and is a regular contributor to The Rag Blog.]
















Dr. Keister,
Another article I read word for word because it made me remember how a physician should think. We called it "hands on medicine" where we got our own chief complaint from the patient and could watch the patients body language; not from a check box on a piece of paper.
A good history of the chief complaint, a revue of systems and family history then a